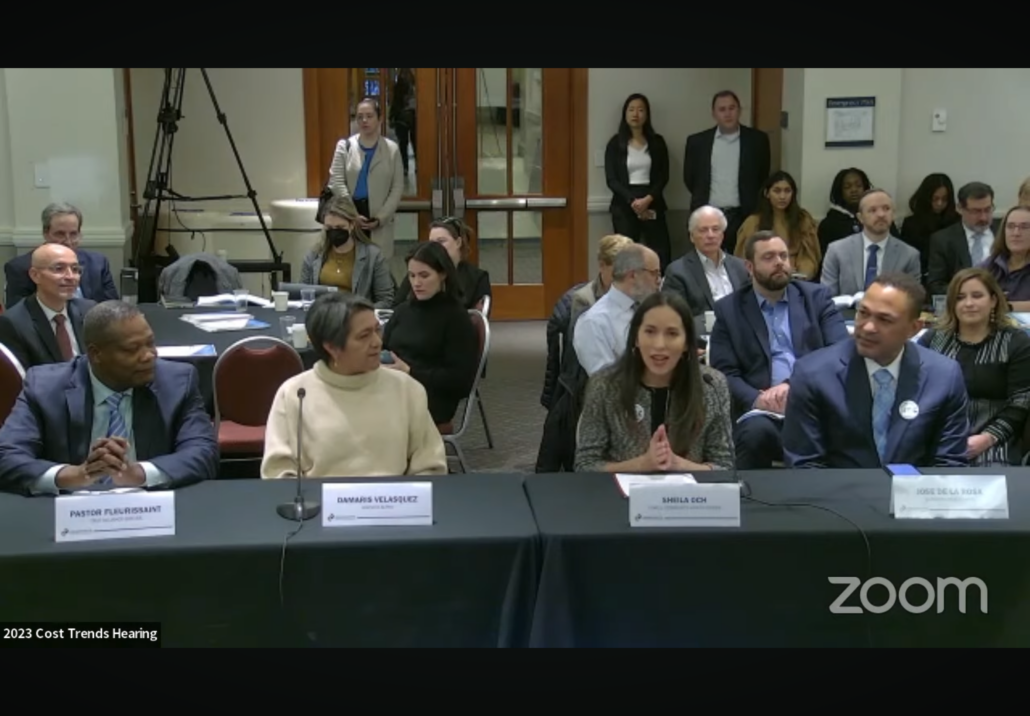
Lowell CHC’s Sheila Och Testifies at the Annual Health Care Cost Trends Hearing
Lowell CHC’s Sheila Och testifying at the Annual Health Care Cost Trends Hearing.
Below is the full text of Sheila’s testimony.
Good Morning. I want to express my gratitude to the organizers for bringing us together for this essential panel. A special thanks to our Attorney General, whose insightful words have set an inspirational tone for our discussions today.
I’m Sheila Och, serving as the Chief Engagement and Equity Officer at Lowell Community Health Center and I also serve as a Community Health Worker and Spanish-speaking Medical Interpreter. I am also a proud member of the Health Equity Compact, a coalition of over 80 leaders of color from various sectors in Massachusetts, united to advance health equity in our state.
I am here today to share my community perspective on the Commission’s recommendations on addressing social determinants of health investments and support for community-led initiatives, and the importance of having a culturally proficient workforce.
As a Community Health Worker in Lowell for over 20 years, I can attest to the impact of initiatives I will be speaking about in a diverse city with the second-largest Cambodian population in the US and half of its population being from the global majority.
Coexisting with this strength and richness, are community health disparities across multiple categories. Systemic racism and historical disinvestment have exacerbated social vulnerabilities, directly impacting health outcomes.
The CDC Social Vulnerability Index sheds light on these disparities in key social determinants of health – such as housing, transportation and poverty. Our census tract has an index score of .82, placing it in the highest vulnerability quartile. Higher index scores are associated with increased healthcare spending and overall health inequities.
Community Health Centers in Massachusetts are innovating to tackle health disparities by creating inclusive and integrated care models while addressing workforce shortages.
Our Metta Health Center, an exemplary initiative, offers holistic care to refugees and immigrants who have experienced trauma, including war and political unrest.
By blending global healthcare approaches and providing primary care, behavioral health services, acupuncture, meditation, and community outreach, Metta patients demonstrate significant improvements in chronic conditions like diabetes, depression, and PTSD.
These success stories emphasize the crucial role of Community Health Centers, expanding care models, and fostering cultural proficiency in healthcare & our workforce.
The Health Policy Commission’s Report emphasizes the significance of supporting and investing in the Commonwealth’s healthcare workforce, with specific mention of CHWs and promotion of workforce diversity.
CHWs play an essential role due to their strong community ties, unwavering empathy, resilience, creativity, skills, and profound respect for their communities. Building trust with the community, particularly within communities of color, involving them in decision-making, and fostering a culturally proficient workforce are paramount for addressing health disparities and ensuring success.
National studies have demonstrated that CHW programs yield an average savings of $2,245 per patient served. These programs not only improve health outcomes for patients and communities but also provide significant financial benefits.
Our Asthma Project, which I was involved in, helps illustrate this. Our project aimed to improve living conditions for low-income families with asthmatic children, resulting in an 81% reduction in emergency room visits for the 239 kids within the program.
The same is true for our older adults in the program. In 2017, a 71-year-old patient joined Asthma program, struggling with uncontrolled asthma that frequently necessitated urgent care visits. The CHW recognized his commitment and via our integrated care approach, the CHW provided him with a spacer for his inhaler, which made an immediate difference, along with practical tools like a HEPA vacuum and allergen-proof bedding and a personalized Asthma Action Plan. Years later, the patient and CHW reunited in October 2023, acknowledging the program’s impact on his quality of life. He now enjoys time with his grandchildren, free from asthma attacks, demonstrating the enduring impact of equity-centered interventions.
The project’s success is due to our dedicated CHWs who conducted home assessments, educational visits, and provided essential resources.
This one single intervention could save our health system over half a million dollars. However, despite all this evidence, securing adequate funding remains a challenge due to historical lack of reimbursement and investments. Consistent financial backing is needed, as our current support relies on a patchwork of grants from various sources.
The Commission’s report provides actionable solutions for strengthening the workforce, connecting with communities, restoring trust in healthcare, and promoting thriving communities. It emphasizes addressing social determinants of health, promoting innovative strategies, and investing in our healthcare workforce.
The Health Equity Compact priorities echo these recommendations, emphasizing investments in public health workforce infrastructure and Health Equity Zones to empower community-led health initiatives.
In closing – As one of our patients stated “I’ve had depression all my life, but thanks to the help and support I’ve received from Lowell CHC, I’ve been able to raise my children and live a normal life. I consider myself one of the lucky ones.”
This is 2023 and getting access to care like this shouldn’t be about luck in a state like ours that has already done so much to advance health care.
We have a moral obligation to address disparities and inequities in health, and our state has the opportunity to lead the way once again.
Our objective is to give everyone an opportunity for a healthy life. I think this is something everyone in this room can agree with.
To make this happen we need let go of traditional healthcare funding models and invest in doing things differently.
It’s time to turn our awareness into impactful action.
To echo our community – What we need now is the courage to make necessary decisions.
Thank you.


